Following the emergence of COVID-19 in Maryland, the University of Maryland Medical System (UMMS) enacted a Strict Patient Safety Policy at all 13 System hospitals, including UM Shore Medical Centers at Chestertown, Dorchester and Easton, on March 20. Hospitals and their health care providers are now faced with a unique challenge most had never experienced before: How do you connect patients with loved ones when visitors are not allowed in your facilities?
UMMS and UM Shore Regional Health (UM SRH) are enforcing a policy that is in the best interest of their team members and their communities. While the updated policy’s intent is to keep patients and hospital team members safe from exposure to COVID-19, few would deny the impact on patient-centered care that the new restrictions pose.
UM SRH values the support of family in the recovery of our patients. Jo Anne Thomson, director of Patient Experience, knows from personal experience how stressful it is for family to be separated from a loved one while they are in the hospital.
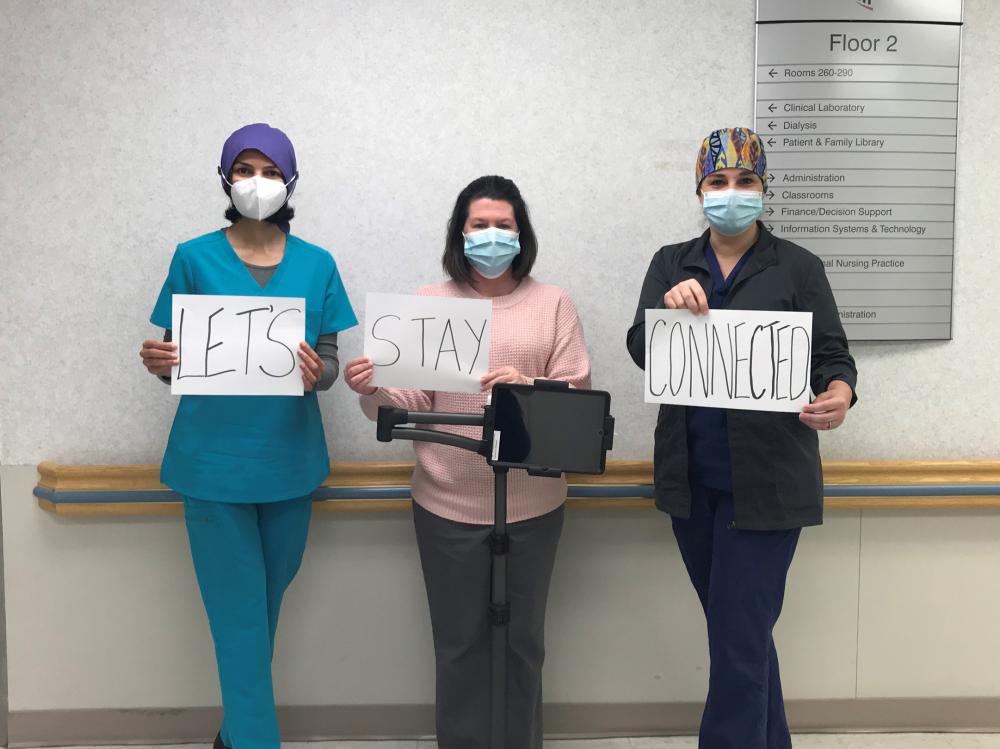
According to Thomson, UM SRH took immediate action to bring patients and families together using video-conferencing technology. When the new visitor policy went into place, Thomson pushed to have video-conferencing software added to iPads and laptops so patients and families could communicate, ensuring these technologies were available as soon as possible to reduce patient and family stress.
Elizabeth “Bee” Fish, director, Information Services and Technology at UM SRH, then connected UM Shore Medical Centers at Chestertown, Dorchester and Easton, as well as the UM Shore Emergency Center at Queenstown with the new software. Thomson worked with clinical teams at all sites, including telemetry, intensive care, palliative care, clinical nurse educators and the Birthing Center at UM Shore Medical Center at Easton to provide education about the need to connect patients and families and about how to use the new video-conferencing software to meet that need.
“We began thinking creatively about connecting our patients to their loved ones, leveraging the technology we have,” Fish said. “We did this because we know how important a visit from a loved one is. Many patients look forward to this and it helps us provide patient-centered care. By using video-conferencing technology, our providers also keep loved ones informed on care their family member is receiving while in the hospital.”
L-R: Lakshmi Vaidyanathan, MD, medical director, SR Palliative Care Program and Population Health; Sarah Hopkins, LCSW-C, social worker, UM SR Palliative Care Program; and Christina Ball, AGACNP, nurse practitioner, UM SR Palliative Care Program.
According to Jeannine Lemieux, clinical nurse educator at UM Shore Medical Center at Easton, these virtual visits help also to reduce patients’ losing sight of their health care goals.
“When I made the offer to my patient to help her connect face-to-face with her family, her eyes lit up and a smile came across her face. We then contacted her granddaughter and her grandson. Such a feeling of joy and peace entered the room when they were able to set eyes on each other. It didn’t matter that they weren’t physically there, they were able to talk and see each other, and that’s all that mattered,” Lemieux said.
Christina Ball, nurse practitioner with UM Shore Regional Health’s Palliative Care Program, said restrictions on visitation cause patients with acute and chronic illness, as well as their families, to face more uncertainty than ever before.
“As a palliative care nurse practitioner, I see that effective patient- and family-centered communication is so important to delivering quality care. New video technologies have provided an avenue to restore that connection for patients and their families during COVID-19,” Ball said.
In Ball’s observation, stress and anxiety have reached new levels. “Not being able to see loved ones in person added significant challenges on multiple levels,” she said.
“By utilizing video chat, we have been able to close this gap for patients and families,” Ball said. “This platform has allowed our team to build trust, alleviate anger, minimize fear, provide reassurance, and in some circumstances, provide closure. We are finding that by providing face-to-face connection, it is alleviating some of the unimaginable burden that has been placed on patients and families because of the no-visitor policy made necessary by COVID-19.”
As a result, she said, patients and families are able to focus on clinical information provided, individualized goals, wishes and necessary steps to move the plan of care forward.
But it doesn’t stop there. There are two other reasons why this technology is even more important during the COVID-19 pandemic: helping UM Shore Medical Group doctors and advanced practice providers monitor and support their patients through telehealth, and observing and communicating with patients who are in isolation units due to a COVID-positive diagnosis.
“When PPE (personal protective equipment) is limited, it is vital to reduce unnecessary contact between clinical staff and COVID-positive patients,” Fish said. “Where assessment of, say, pain levels, is the goal and physical touch is not necessary, we can lessen contact for clinical team members who may not need to physically enter the room.”
More information about UMMS and UM SRH’s response to COVID-19 is available on the System’s dedicated COVID-19 information webpage, https://www.umms.org/covid.
As part of the University of Maryland Medical System (UMMS), University of Maryland Shore Regional Health is the principal provider of comprehensive health care services for more than 170,000 residents of Caroline, Dorchester, Kent, Queen Anne’s and Talbot counties on Maryland’s Eastern Shore. UM Shore Regional Health’s team of more than 2,200 employees, medical staff, board members and volunteers works with various community partners to fulfill the organization’s mission of Creating Healthier Communities Together.
Don’t miss the latest! You can subscribe to The Chestertown Spy‘s free Daily Intelligence Report here


Write a Letter to the Editor on this Article
We encourage readers to offer their point of view on this article by submitting the following form. Editing is sometimes necessary and is done at the discretion of the editorial staff.