As opioid deaths in Maryland remain a public health crisis, a Centreville doctor is calling for decriminalization and a public health approach to addiction modeled on successful reforms in other parts of the world.
Dr. Eric Ciganek, who treats recovering opioid patients in his Centreville practice, said the U.S spends “billions of dollars” a year on drug enforcement “because it’s the only thing we know.”
“In 1971 Richard Nixon announced the war on drugs, do you think we won?” he asked rhetorically during an interview with the Spy. “We lost terribly.”
Ciganek proposes a decriminalization model similar to Portugal, “where the rates of addiction, overdose and infectious diseases have dropped dramatically.”
Overdose deaths, disease transmission and drug related incarcerations fell after Portugal decriminalized drug use in 2001. Overall drug use declined and voluntary participation in treatment programs increased, contrary to the fears of opponents at the time.
“The amount of people in jail has dropped dramatically and the amount of people going in front of judges…has dropped dramatically,” Ciganek said.
He said 75 percent of the inmates in the Queen Anne’s County Detention Center are there for nonviolent crimes committed to support their habit, like shoplifting and breaking and entering.
Safe Injection Sites
Ciganek said medically supervised injection sites would lower overdose mortality and reduce the spread of Hepatitis C and other infectious diseases.
He said there’s a crisis looming with Hepatitis C — when years from now many addicts and former addicts will develop liver cancer.
“We have a national disaster on our hands that we’re not even looking at,” he said. He said people can live up to 25 years without knowing they have Hepatitis C.
There are about 100 injections sites in 66 cities around the world. Users bring their own drugs and inject themselves in a medically supervised environment with clean syringes provided by the facility. Denmark, France, Germany, Luxembourg, Netherlands, Norway, Spain, Switzerland, Australia, and Canada all have safe injection sites. The results in these countries also show reduction in overdose deaths and an increase in transition to treatment.
There are currently no sanctioned injection sites in the U.S, and recent attempts to establish them have come with a warning from the Department of Justice.
“Because federal law clearly prohibits injection sites, cities and counties should expect the Department of Justice to meet the opening of any injection site with swift and aggressive action,” wrote Deputy Attorney Rod Rosenstein in the New York Times in 2018.
Rosenstein kept his word; in February the U.S. Attorney for the Philadelphia William McSwain sued to stop SafeHouse in Philadelphia from opening the first injection site in the U.S.
In a hearing on Sept. 5, McSwain argued that SafeHouse would violate the federal “crack house” statute that prohibits maintaining a place for drug use.
Current treatment options
Ciganek favors Suboxone with buprenorphine as a primary treatment method in his practice.
“It’s a weak opiate with almost no euphoric properties but it stimulates an opiate receptor in the brain that prevents a patient from going into withdrawal.” He said it eliminates cravings and is “well tolerated” if patients us it correctly.
Vivitrol is another treatment, a shot given that stops the effects of opioids for a month.
“It will prevent people from getting high,” he said. “It sits on an opiate receptor in the brain and blocks it.”
Ciganek favors the use of Vivitrol before patients leave rehab or prison because detoxification will have already occurred. To avoid withdrawal symptoms, there can be no opiates in the system when the shot is administered. He said almost 90 percent will use drugs within 48 hours of leaving a facility.
Vivitrol has also found its way to the court system, allowing patients to take it voluntarily as a condition of probation to avoid prison or get a reduced sentence.
MD Death toll rises in 2017 – 2018, tapers off in first quarter of 2019
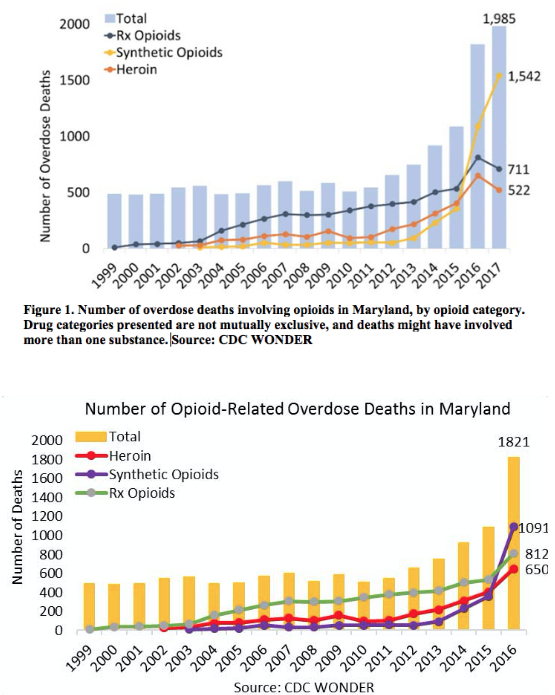
There were 1,985 opioid deaths in Maryland in 2017, or 32 deaths per 100,000 of population, more than twice the national average, according to CDC data. This ranked Maryland fifth in the U.S for overdose deaths.
The majority of the deaths, 1,542, were from fentanyl, nearly a 30 percent increase over 2016. Prescription opioids and heroin deaths declined to 711 and 522 respectively from 2016, but the spike in fentanyl deaths in 2017 raised the state’s opioid death rate by 8 percent over 2016. (See figures 1 and 2)
Kent County had three fentanyl related deaths in 2017, one from heroin and two from prescribed opioids, according to Maryland Health Department records. There were two deaths in 2018, both attributed to fentanyl.
A 2018 report from the Maryland Opioid Operational Command Center showed another increase in the death toll to 2,114. And while the report indicated another decline in prescription opioid and heroin deaths, it cautioned that the declines “may be the result of displacement of heroin for fentanyl as the drug of choice for many users.”
The first quarter of 2019 marked a decline from the first quarter of 2018 statewide, a drop in 86 deaths, from 601 to 515, according to an OOCC report released in June. Fentanyl related deaths declined by 8 percent over the same period last year. Prescription opioid deaths dropped by 23 percent and heroin deaths dropped 16 percent.
But Kent County has gone in the opposite direction with seven deaths occurring so far this year, three in the first quarter and four in the second — all of them are attributed to fentanyl, said Joe Jones, the local addictions authority with the Kent County Health Department.
Fentanyl’s rise as the drug of choice grew out of shortages of heroin and greater difficulty obtaining opioid prescriptions, said a recent report from University of California San Francisco. “It is about 30 to 40 times stronger than heroin and considerably cheaper to produce.”
Ciganek believes the decline in opioid prescribing fueled the rise of overdose deaths as more addicts switched to fentanyl.
“When people were doing Oxycodone they weren’t dying as much as they are now,” he said.




Joy says
Suboxone works but only if taken as you are suppose to, but nothing will work if your not truly ready to stop. When you start the first step you can have No Reservations. If you go the suboxone route you also needs to go to meetings and work the steps and live by the traditions. You know when your ready to stop. You go after your recovery like you went after drugs. It’s not easy if you truely work the program but it’s ALOT EASIER then living the drug life. When your sick and tired of being sick and tired and want to change find a meeting they are everywhere. Remember ” NOTHING CHANGES IF NOTHING CHANGES ” God speed
James Bogden says
Good article – I appreciate seeing the data. It’s time to make this happen!